
Helpful Resources
The following resources have been developed to help individuals and families understand how to prepare for Medicaid renewal and what to expect during and after eligibility checks.





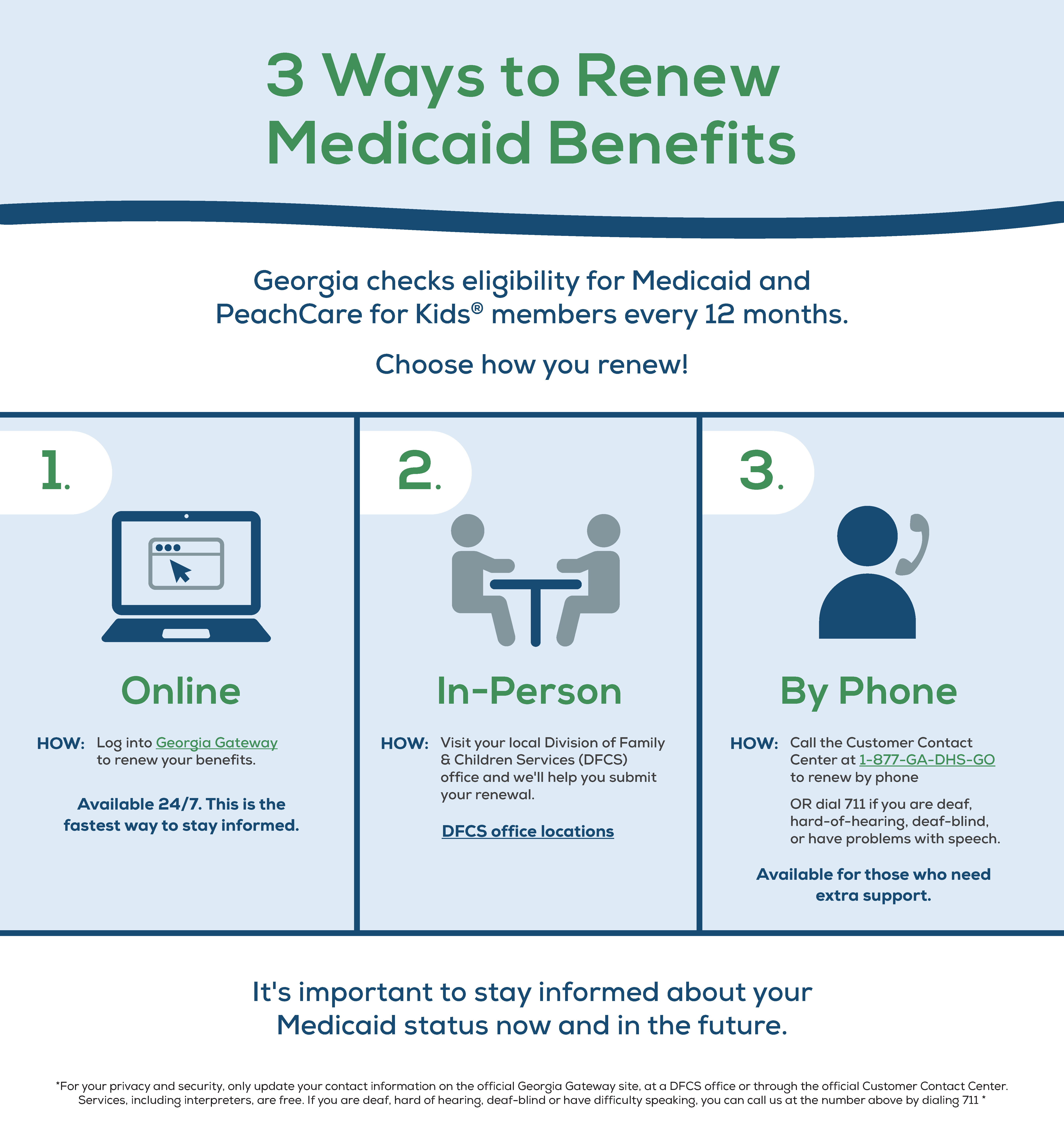
Renewal is the process that the State of Georgia must follow to make sure current Medicaid and PeachCare for Kids® members are still eligible for coverage. Both Medicaid and PeachCare for Kids® benefits require renewals every 12 months.
During renewal, the State of Georgia will collect and verify your information, including income and contact details, as well as other requested information or documents that they’ll use to determine your eligibility.
Log into your Gateway account at gateway.ga.gov to ensure your notices are going to the correct mailing address or to the email that you check regularly. You want to be sure you can be reached with information about your case and that you can find out the date when your renewal is due. As you prepare, you can find more information about your renewal deadline by logging into your Gateway account.

Once you are assigned your renewal date in Gateway, you will receive a letter in the mail or an email with a renewal form and additional instructions.
Be on the lookout for an official letter or an email from the Georgia Department of Human Services (DHS) letting you know that your renewal process has begun. The letter will explain that your renewal window has begun, and that you may have to submit documents like pay stubs or other materials to complete your renewal. Keep track of dates and any requested documents.
If DHS has not heard or received documentation from you after a month, you will get a reminder letter or an email that your coverage eligibility decision is coming soon. Prepare and submit any requested documents as soon as possible to avoid a potential gap in coverage.
This is the date that all your paperwork must be submitted in Gateway or in person to the DHS. If you are found eligible, this is your Medicaid or PeachCare for Kids® renewal date. If you are no longer eligible, this is your coverage expiration date; you will be connected to other health care program options on Georgia Access. If you missed the deadline, you still have 90 days from your renewal date to submit the proper paperwork and potentially regain coverage.
If you were denied coverage for any reason other than “failing to submit” paperwork on time, and feel that an error was made, you can appeal the decision by asking for a Fair Hearing. If you want to keep getting coverage while you wait for the fair hearing decision, you need to check the “I want to continue receiving benefits” box on the form at the end of the denial letter and send in the form within 14 days of denial.
If a member has aged out of PeachCare for Kids® or is no longer eligible for Medicaid, DHS will refer members to to Georgia Access for alternative coverage options.
If you were denied coverage for any other reason other than “failing to submit” paperwork on time and feel that an error was made, you can appeal the decision by asking for a Fair Hearing, but it must be requested either verbally with a case worker or in writing within 30 days of your denial date.
If a member has aged out of PeachCare for Kids® or is no longer eligible for Medicaid, DHS will refer members to Georgia Access for alternative coverage options.
The best way to get information about your Medicaid coverage and other benefits is through the Gateway online portal. When you visit gateway.ga.gov, please scroll to find the following options:
Once you’ve accessed your account, you have the option to choose how you would like to get notifications about your Medicaid renewal status. Choose “email” to get fastest and most convenient updates online.
If you choose “email,” please enter your email address to get timely notifications. NOTE: If your immediate family members/children are covered by Medicaid or PeachCare for Kids® and have an account on Georgia Gateway, please make sure you list the same primary email address for each member of your family.
When updating your Gateway account, be sure to complete all required fields.
To protect your privacy, anyone who helps you with your Medicaid or PeachCare for Kids® coverage must be approved as an “Authorized Representative” for your case.
Authorized Representatives, like a trusted family member, friend, or provider, must have your permission to receive information about your case or to make decisions on your behalf.
If someone has power of attorney for a member, that person still needs to go through the separate process of being added as an Authorized Representative.


Once your Medicaid renewal window has begun, you’ll need to follow the instructions listed in the notification letter or email you received. It’s important to submit your documents as soon as you can to help avoid a gap in your coverage.
The fastest way to submit information is to visit gateway.ga.gov. Visit your local public library for easy Gateway access using the free self-service benefits kiosks. See a map of kiosk locations here. Or, you can mail, fax or bring hard copies of your paperwork to the local Division of Family & Children Services office. You can also call 1-877-423-4746 and complete the process over the phone through the automated system.
If you are no longer eligible for Medicaid, you will be connected to other health care program options on Georgia Access. Below are several alternative options for coverage:
If you were denied for any other reason, you have the option to appeal that decision if you believe that the denial decision is in error. You have 30 days from the denial date to ask for a Fair Hearing to appeal the decision.
To request a Fair Hearing, members should fill out and submit the “Fair Hearing Request” form at the end of their denial letter and send it back to their local Department of Family and Children Services office.
If you want to keep coverage while you wait for a Fair Hearing decision, you need to check the “I want to continue receiving benefits” box on the form and send in the form within 14 days of denial.
The Office of State Administrative Hearings, called OSAH, handles reviews of cases. When your hearing has been scheduled, you will receive a notice in the mail with the time and location of your hearing. At your hearing, you will be able to share why you think you are still eligible for Medicaid/PeachCare for Kids®.
You can help your case by bringing and presenting documents like receipts and bills that help explain your income status.
If the judge reinstates your benefits after the Fair Hearing, your coverage will be made active back to the date of your original determination – so you can get coverage for the medical expenses that you had in the meantime.